Case Study 16 - CC: 2 brief episodes of vision loss in the R eye
Patient Visit
Diagnosis and Discussion
Self-Assessment Questions
Self-Assessment Answers
����ӰԺ Ophthalmology and Visual Sciences Case Studies
-
Ophthalmic Case Study 1
Acute right eye pain -
Ophthalmic Case Study 2
Red, itchy eyes -
Ophthalmic Case Study 3
Acute left eye pain and blurry vision -
Ophthalmic Case Study 4
Left eye pain and fuzzy vision 2 days after eye surgery -
Ophthalmic Case Study 5
Girl rubbing her R eye after trauma -
Ophthalmic Case Study 6
Red eye and pain on the left -
Ophthalmic Case Study 7
Vision loss L eye -
Ophthalmic Case Study 8
Crossed eyes -
Ophthalmic Case Study 9
White pupils -
Ophthalmic Case Study 10
Blurry vision in the left eye for 2 weeks -
Ophthalmic Case Study 11
Acute pain and burning in L eye -
Ophthalmic Case Study 12
Blurry vision in both eyes and headaches -
Ophthalmic Case Study 13
"Cannot see well" from left eye -
Ophthalmic Case Study 14
Blurry vision in both eyes -
Ophthalmic Case Study 15
Eye irritation and dryness -
Ophthalmic Case Study 16
2 brief episodes of vision loss in the R eye -
Ophthalmic Case Study 17
Routine eye exam -
Ophthalmic Case Study 18
8-year-old boy, difficulty seeing whiteboard -
Ophthalmic Case Study 19
8-year-old girl, wandering eye and double vision. -
Ophthalmic Case Study 20
Red eyelid lesion in an infant
Contact Ophthalmology
For patient care inquires, call us at (414) 955-2020 or use MyChart. Email is for research and education inquiries only.
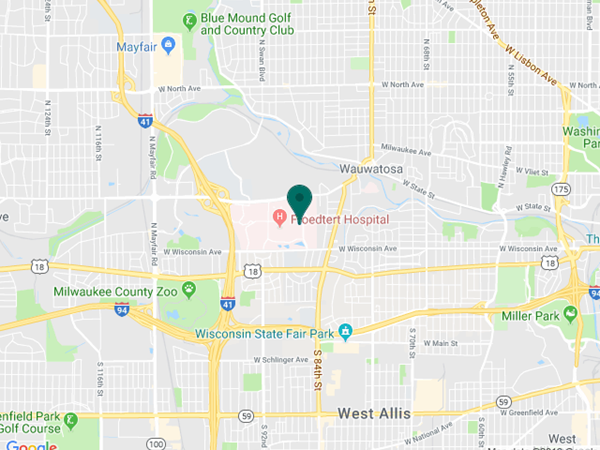
Eye Institute Location
925 N. 87th St.
Milwaukee, WI 53226
Appointments
(414) 955-2020
(414) 955-6166 (fax)
Continuing Medical Education
Amanda Tan
(414) 955-2049
Medical Education Coordinator
Associate Director of Development - Ophthalmology
Sarah Walker
Refer to Us - Consultation requests
Patient Referral Form (PDF)
Fax to (414) 955-0136
Emergent Requests
Within 48 hours call
(414) 955-2020
Research
Vesper Williams
(414) 955-7862
Advanced Ocular Imaging Program
(414) 955-2647
Eye Institute Executive Director (Administrator)
Shannon Dreier